On June 28, 2019, California Governor Gavin Newsom signed into law a state budget for 2019-2020 that establishes a state individual mandate, effective Jan. 1, 2020. This state-based individual mandate will require California residents to maintain acceptable health coverage or pay a penalty, beginning in 2020.
This new mandate was enacted in response to the effective elimination of the federal individual mandate penalty under the Affordable Care Act (ACA). The ACA’s individual mandate penalty was reduced to zero under the Tax Cuts and Jobs Act, beginning in 2019.
State Individual Mandate
Beginning in 2020, California will impose a state individual mandate that largely mirrors the ACA’s federal individual mandate requirement. The ACA’s individual mandate penalty has been effectively eliminated beginning in 2019.
California’s individual mandate will require most individuals in the state (and their family members) to be covered under minimum essential coverage for each month of the year, beginning in 2020. Individuals that don’t obtain acceptable health insurance coverage will be penalized.
Minimum Essential Coverage
For purposes of the California individual mandate, the term “minimum essential coverage” (MEC) generally has the same definition as under the ACA.
The Penalty Amount
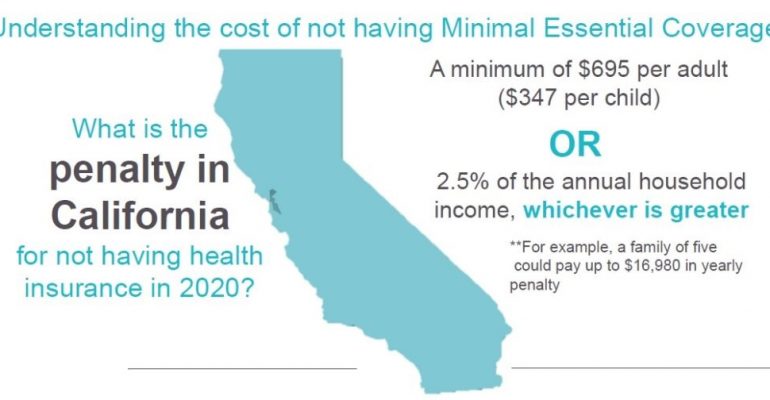
California’s individual mandate penalty is calculated in the same manner as the ACA’s individual mandate. The penalty is the greater of two amounts—the flat dollar amount ($695) or the percentage of income amount (2.5% of income). For purposes of calculating the penalty, income is the taxpayer’s household income for the taxable year over the state income tax filing threshold for the taxable year.
Families will pay half the penalty amount for children, up to a family cap of three times the annual flat dollar amount. Also, the penalty is capped at the California state average of the annual bronze plan premium.
Affected Individuals
The requirement to maintain MEC applies to individuals of all ages (including children), unless that individual falls within a specific exception or is exempt. An individual is treated as having coverage for a month if he or she has coverage for any one day of that month.
The following categories of individuals are exempt from the California individual mandate penalty:
- Individuals who cannot afford coverage;
- Religious conscience objectors;
- Members of a health care sharing ministry;
- Incarcerated individuals;
- Individuals not lawfully present in the United States;
- Members of an Indian tribe;
- Nonresident taxpayers;
- Individuals enrolled in limited or restricted scope coverage under the Medi-Cal program (or of a substantially similar program).
Reporting Requirement
To help administer the individual mandate penalty, the California law imposes a reporting requirement on every entity that provides MEC to an individual during a calendar year, similar to the ACA’s reporting requirement under Internal Revenue Code Section 6055. This reporting requirement applies to:
- Employers or other sponsors of employment-based health plans, for employment-based MEC;
- The State Department of Health Care Services and county welfare departments, for MEC under a state program;
- Carriers licensed or otherwise authorized to offer health coverage, for MEC they provide that is not described above (including catastrophic plan coverage);
- The Exchange, for individual health plans (except catastrophic plans) on the Exchange; and
Any other provider of MEC (including the University of California, for coverage under a student health insurance program).
Under this reporting requirement, entities that provide MEC will be required to provide the following information to covered individuals and the California Franchise Tax Board by March 31 of each year:
- The name, address and Social Security number (SSN) or taxpayer identification number (TIN) of the primary insured, and the name and SSN or TIN of each other individual covered under the policy;
- The dates during which those individuals were covered under MEC during the calendar year; and
- Any other information the Franchise Tax Board may require.
The new law specifically provides that the California reporting requirement may be satisfied by providing the same information that is currently reported under the federal Section 6055 reporting requirement.